An overview of Deep Vein Thrombosis
What is Deep Vein Thrombosis?
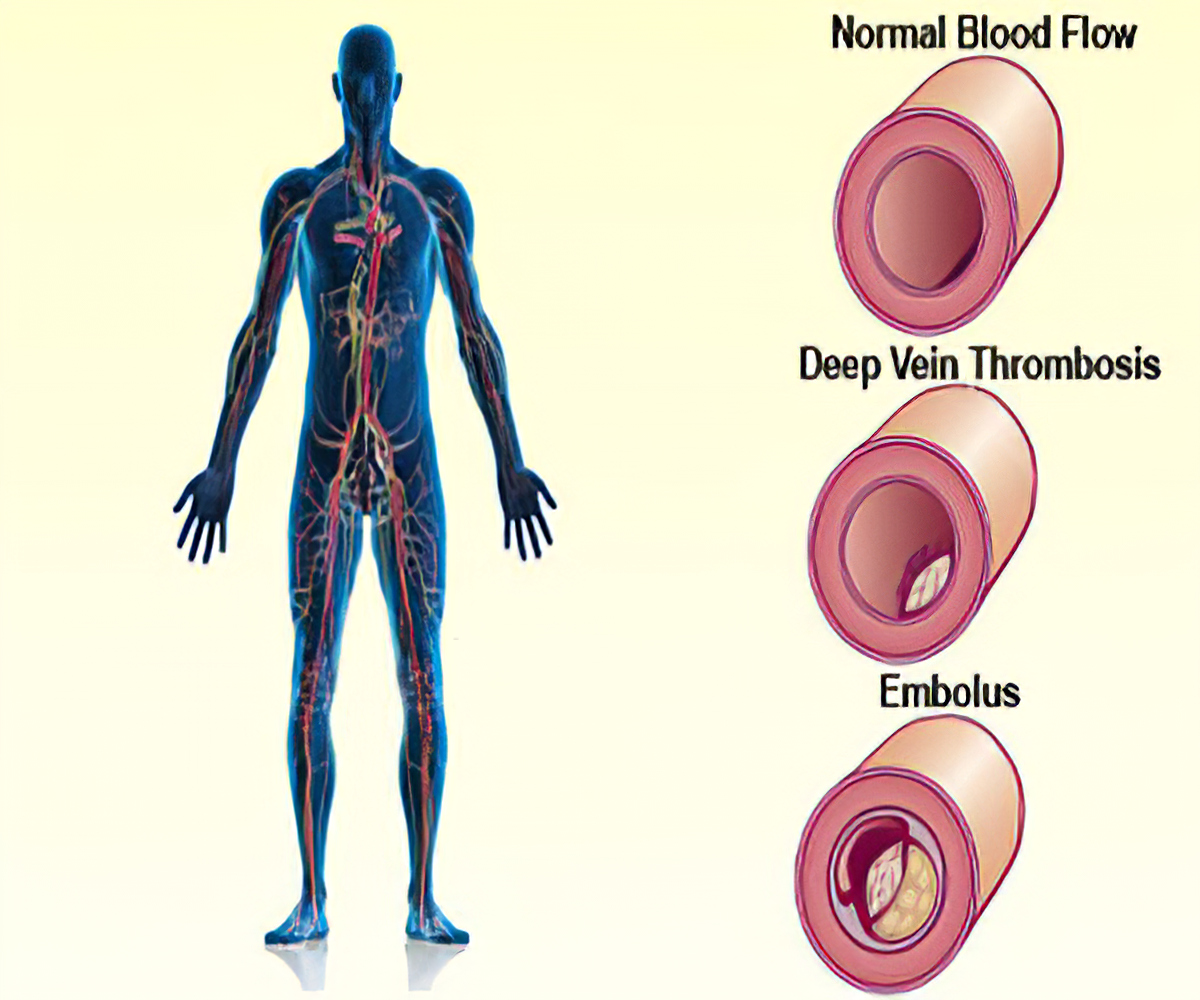
Deep vein thrombosis occurs when a thrombus (blood clot) develops in veins deep in your body because your veins are injured or the blood flowing through them is too sluggish. The blood clots may partially or completely block blood flow through your vein. Most DVTs happen in your lower leg, thigh or pelvis, but they also can occur in other parts of your body including your arm, brain, intestines, liver or kidney.
DVT Management
Activity Guidelines
A DVT may make it harder for you to get around at first because of leg pain and swelling. But you’ll be able to slowly return to your normal activities. If your legs feel swollen or heavy, lie in bed with your heels propped up about 5 to 6 inches. This helps improve circulation and decreases swelling.
In addition:
1. Exercise your calf muscles if you’re sitting still for long periods of time.
2. Stand up and walk for a few minutes every hour while awake and especially during a long-haul flight or road trip.
3. Wear knee-high compression stockings. These minimize leg pain and swelling by at least 50% if you wear them daily.
4. Avoid activities that may cause a serious injury.
5. Stay hydrated at all times, and especially during travel.
Causes of deep vein thrombosis
These conditions can increase your risk of a deep vein thrombosis:
1. Having an inherited (genetic) condition increases your risk of blood clots.
2. Having cancer and some of its treatments (chemotherapy).
3. Having a history of deep vein thrombosis in yourself or your family.
4. Having limited blood flow in a deep vein because of an injury, surgery or immobilization.
5. Not moving for long periods of time, like sitting for a long time on trips in a car, truck, bus, train or airplane or being immobile after surgery or a serious injury.
6. Being pregnant or having recently delivered a baby.
7. Being older than 40 (although a DVT can affect people of any age).
8. Having overweight/obesity.
9. Having an autoimmune disease, like lupus, vasculitis or inflammatory bowel disease.
10. Using tobacco products.
11. Having varicose veins.
12. Taking birth control pills or hormone therapy.
13. Having a central venous catheter or pacemaker.
14. Having COVID-19.
Risk factors of DVT
Many things can increase the risk of developing deep vein thrombosis. The more risk factors you have, the greater your risk of DVT. Risk factors for DVT include:
1. Age.Being older than 60 increases the risk of DVT. But DVT can occur at any age.
2. Lack of movement.When the legs don't move for a long time, the calf muscles don't squeeze (contract). Muscle contractions help blood flow. Sitting for a long time, such as when driving or flying, increases the risk of DVT. So does long-term bed rest, which may result from a lengthy hospital stay or a medical condition such as paralysis.
3. Injury or surgery.Injury to the veins or surgery can increase the risk of blood clots.
4. Pregnancy.Pregnancy increases the pressure in the veins in the pelvis and legs. The risk of blood clots from pregnancy can continue for up to six weeks after a baby is born. People with an inherited clotting disorder are especially at risk.
5. Birth control pills (oral contraceptives) or hormone replacement therapy.Both can increase the blood's ability to clot.
6. Being overweight or obese.Being overweight increases the pressure in the veins in the pelvis and legs.
7. Smoking.Smoking affects how blood flows and clots, which can increase the risk of DVT.
8. Cancer.Some cancers increase substances in the blood that cause the blood to clot. Some types of cancer treatment also increase the risk of blood clots.
9. Heart failure.Heart failure increases the risk of DVT and pulmonary embolism. Because the heart and lungs don't work well in people with heart failure, the symptoms caused by even a small pulmonary embolism are more noticeable.
10. Inflammatory bowel disease.Crohn's disease or ulcerative colitis increase the risk of DVT.
11. A personal or family history of DVT or pulmonary embolism (PE).If you or someone in your family has had one or both of these conditions, you might be at greater risk of developing DVT.
12. Genetics.Some people have DNA changes that cause the blood to clot more easily. One example is factor V Leiden. This inherited disorder changes one of the clotting factors in the blood. An inherited disorder on its own might not cause blood clots unless combined with other risk factors.
Sometimes, a blood clot in a vein can occur with no identifiable risk factor. This is called an unprovoked venous thromboembolism (VTE).
Signs and symptoms of deep vein thrombosis
A DVT usually forms in the veins of your legs or arms. Up to 30%of people with a DVT don’t have symptoms, but sometimes the symptoms are very mild and may not raise concern. The symptoms associated with an acute DVT include:
1. Swelling of your leg or arm (sometimes this happens suddenly).
2. Pain or tenderness in your leg or arm (may only happen when standing or walking).
3. The area of your leg or arm that’s swollen or hurts may be warmer than usual.
4. Skin that’s red or discolored.
5. The veins near your skin’s surface may be larger than normal.
6. Abdominal pain or flank pain (when blood clots affect the veins deep inside your abdomen).
7. Severe headache (usually of sudden onset) and/or seizures (when blood clots affect the veins of your brain).
Some people don’t know they have a DVT until the clot moves from their leg or arm and travels to their lung. Symptoms of acute PE include chest pain, shortness of breath, cough with blood, lightheadedness and fainting.
It’s important to call your doctor right away or go to the emergency room if you have symptoms of a DVT. Don’t wait to see if your symptoms go away. Get treatment right away to prevent serious complications.
Preventive measures against DVT
After you have a DVT, you’ll need to reduce your risk of future DVT/PE clots by:
1. Taking your medications exactly as your healthcare provider tells you to.
2. Keeping your follow-up appointments with your doctor and the laboratory. These tell your provider how well your treatment is working.
3. Making lifestyle changes, such as eating healthier foods, being more active and avoiding tobacco products.
If you’ve never had a DVT, but have an increased risk of developing one, be sure to:
1. Exercise your calf muscles if you need to sit still for a long time. Stand up and walk at least every half hour if you’re on a long flight. Or get out of the car every hour if you’re on a long road trip.
2. Get out of bed and move around as soon as you can after you’re sick or have surgery. The sooner you move around, the less chance you have of developing a DVT.
3. Take medications or use compression stockings after surgery (if your provider prescribes them) to reduce your risk of a clot.
4. Follow up with your provider as directed and follow their recommendations to reduce your risk of a clot.
DVT Diagnosis and Tests
How is DVT diagnosed?
Your healthcare provider will do a physical exam and review your medical history. You’ll also need to have imaging tests.
Tests to diagnose a DVT
1. Duplex venous ultrasound.This is the most common test for diagnosing a DVT because it is non-invasive and widely available. This test uses ultrasound waves to show blood flow and blood clots in your veins. A vascular ultrasound technologist applies pressure while scanning your arm or leg. If the pressure doesn’t make your vein compress, it could mean there’s a blood clot. If the results of the duplex ultrasound aren’t clear, your provider can use another imaging test
2. Venography. In this invasive test, your provider numbs the skin of your neck or groin and uses a catheter to inject a special dye (contrast material) into your veins to see if any blood clots are partially or completely blocking blood flow inside your veins. Venography is rarely used nowadays, but sometimes it is necessary
3. Magnetic Resonance Imaging (MRI) or Magnetic Resonance Venography (MRV).MRI shows pictures of organs and structures inside your body. MRV shows pictures of the veins in specific locations in your body. In many cases, MRI and MRV can offer more information than a duplex ultrasound or CT scan.
4. Computed tomography (CT) scanis a type of X-ray that shows structures inside your body. Your provider may use a CT scan to find a DVT in your abdomen, pelvis or brain, as well as blood clots in your lung (pulmonary embolism).
If your doctor thinks you may have a genetic or acquired clotting disorder, you may need to have special blood tests. This may be important if:
1. You have a history of blood clots that your provider can’t link to any other cause.
2. You have a blood clot in an unusual location, such as in a vein from your intestines, liver, kidney or brain.
3. You have a strong family history of blood clots.
4. You have a family history of a specific genetic clotting disorder.
Treatment for DVT
Some people with a DVT may need to be treated in the hospital. Others may be able to have outpatient treatment.
Treatments include medications called anticoagulants (blood thinners), compression stockings and elevating your affected leg(s) at different times throughout the day. In a minority of cases, when the DVT is extensive, invasive treatments (catheter-based procedures) may be required.
The main goals of treatment are to:
1. Keep the clot from getting bigger and involving other veins.
2. Prevent the clot from breaking off in your vein and moving to your lungs.
3. Lessen the risk of another blood clot.
4. Prevent long-term complications from the blood clot (like chronic venous insufficiency).
Important information about medications
1. Take your medications exactly as your healthcare provider tells you to.
2. Have blood tests your provider requests and keep all scheduled laboratory appointments.
3. Don’t stop or start taking any medication (including medications and supplements you take without a prescription) without asking your provider.
4. Talk to your provider about your diet. You may need to make changes, depending on the medication you take.
DVT treatments
Anticoagulants (blood thinners)
This type of medication makes it harder for your blood to clot. Anticoagulants also stop clots from getting bigger and prevent blood clots from moving. Anticoagulants don’t destroy or “melt” blood clots. Your body may naturally dissolve a clot, but sometimes clots don’t completely disappear. When they don’t, they usually shrink and become little “scars” inside your veins. Sometimes these “old” clots may result in leg swelling, but oftentimes they don’t cause symptoms.
There are different types of anticoagulants: warfarin, heparin and oral Xa inhibitors. Your doctor will talk to you about the best type of medication for you.
If you need to take an anticoagulant, you may have to take it for only a few months (usually three to six months) or you might take it indefinitely. Your treatment time may be different depending on the specific situations of each individual, including if:
1. You’ve had clots before.
2. You’re getting treatment for another illness, like cancer or an autoimmune disease (you may need to take an anticoagulant as long as your risk of a clot is higher.).
Bleeding is the most common side effect of anticoagulants. You should call your doctor right away if you notice that you bruise or bleed easily while taking this medication.
Compression Stockings
You‘ll probably need to wear graded elastic compression stockings to either improve or completely get rid of leg swelling. Damage to the small valves inside your veins often causes this swelling. You may also have swelling because the DVT is blocking blood flow in your vein. You wear most compression stockings just below your knee. These stockings are tight at the ankle and become looser as they go away from your ankle. This causes gentle pressure (compression) on your leg. Some people need to wear these for two years or more. Several clinical studies have shown that compression stockings improve the symptoms of leg pain and swelling by at least 50% as long as they’re worn daily from morning to evening (they don’t have to be worn overnight).
After surgery, your providers may put compression devices on your calves to put pressure on them. These machines squeeze and release the fabric-covered devices around your calves while you’re lying in bed. These devices help prevent a DVT if you’re in the hospital, but they aren’t prescribed outside of the hospital. In addition, unlike compression stockings that you can wear safely when a leg DVT is present, you shouldn’t use these devices for DVT prevention if you have a DVT.
DVT Treatment Procedures
When you can’t take medications to thin your blood or you have blood clots while taking blood thinners without missing doses, a surgeon may have to do a procedure to put in an inferior vena cava (IVC) filter. The procedure is done under local anesthesia. Your surgeon inserts the IVC filter through a catheter into a large vein in your groin or neck, and then into your vena cava (the largest vein in your body). If blood clots in the veins of your legs break off and travel, the IVC filter is designed to prevent large blood clots (emboli) from reaching your lungs and causing a pulmonary embolism. While an IVC filter helps prevent a pulmonary embolism, it doesn’t keep more blood clots from forming in your veins.
Complications
1. Pulmonary embolism (PE).PE is a potentially life-threatening complication associated with DVT. It occurs when a blood clot (thrombus) in a leg or other body area breaks free and gets stuck in a blood vessel in a lung.
Get immediate medical help if you have symptoms of PE. They include sudden shortness of breath, chest pain while breathing in or coughing, rapid breathing, rapid pulse, feeling faint or fainting, and coughing up blood.
2. Postphlebitic syndrome.Damage to the veins from the blood clot reduces blood flow in the affected areas. Symptoms include leg pain, leg swelling, skin color changes and skin sores.
3. Treatment complications.Blood thinners are often used to treat DVT. Bleeding (hemorrhage) is a worrisome side effect of blood thinners. It's important to have regular blood tests while taking blood-thinning drugs.
Frequently Asked Questions About DVT
In general, treatment for deep vein thrombosis is successful without serious complications and the body can return to normal function. The condition, however, can recur, so precautionary measures to reduce risk as much as possible are advisable. Chronic occurrence of post-phlebitic syndrome can lead to long-term oedema (swelling) or pain which will need to be carefully managed by a treating doctor.
Blood stasis, procoagulant tendency, and endothelial injury. Each of these can lead to thrombosis.
It is not known whether a below-knee DVT confers increased risk of PE; it is certainly a common incidental finding in otherwise well individuals.If local symptoms are thought to be due to the DVT, offer treatment. If not, consider repeat scanning in one week to see if the clot has extended proximally.
Those aged more than 55yrs with unprovoked DVT, and those with recurrent unprovoked DVT or DVT at an unusual site.